
I have been very active representing EMS interests in public safety communications, such as FirstNet, for the past 18 years. I am now working with police, fire and 911 colleagues on the Public Safety NG911 Coalition to promote the major build-out of Next Generation 911 services around the country to round out emergency response capabilities anchored by FirstNet. There have been multiple efforts to do this in the recent past, with associated bills failing in Congress. The Public Safety NG911 Coalition is using the opportunity presented by the COVID-19 crisis and Congressional response to build infrastructure to address this and future threats. Upcoming COVID-19 or related legislation will hopefully contain language funding $15 billion to widely establish NG911 system capabilities across the US.
This suggests opportunities for EMS in general and community paramedicine and rural EMS in particular. If you haven’t read my blog on EMS Concerns for the Here and Now related to this topic, take a look.
At the turn of the millennium, when community paramedicine (CP) got its name, we mined the earlier Red River, New Mexico “pilot” results and other adaptive uses of EMS professionals for lessons and opportunities. Twenty years later, CP and mobile integrated healthcare (MIH) have become well-accepted practices and not just fads. Yet, even just a couple of years ago, when virtually every state was contemplating CP and well over 200 communities were experiencing it, we all wondered how it could be a sustainable model.
Ironically, CP started as a rural concept. We thought that enabling advanced EMS professionals to provide and be reimbursed for scarce non-emergency patient care in a community might create the critical mass to fund the presence and skills retention for a paramedic or advanced EMT to be available for emergencies in a low-volume setting far from the nearest hospital…a resource otherwise unavailable to that rural community. That model has certainly come to pass to some degree in many rural communities. The irony, though, is found in the success of urban applications of CP that have the numbers to begin to prove the value of the concept and the healthcare resources to channel funding to promising CP-MIH applications. They far outstrip the patient contacts of CP in rural communities.
We have seen progress in the sustainability of CP-MIH type services. From the revenue they produce in high volume health system contracts to reimbursement for CP services by large health insurance companies in 14 states, the sustainability scale is tipping in the right direction. The key for the future is pushing the healthcare funding establishment away from the perverse incentives it has created for EMS: demanding that EMS transport patients to a hospital emergency department (ED) to be paid for services rendered.
The Centers for Medicare and Medicaid Services (CMS) Emergency Triage, Treat and Transport (ET3) pilot also specifically moves in this direction, estimating that 16% of ambulance transports to an ED could be routed to less expensive care, saving $560 million per year (see CMS diagram below).
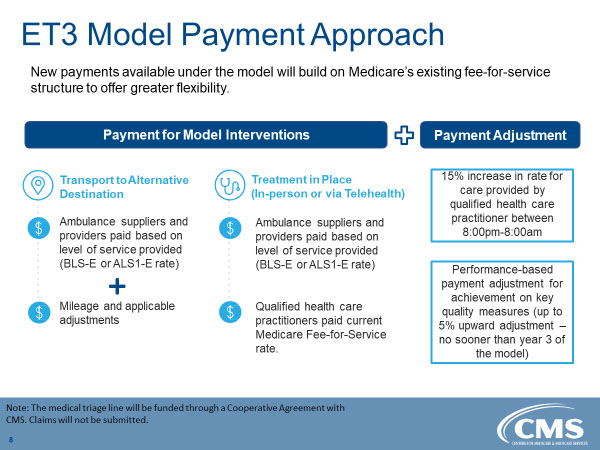
The ET3 program offers incentives for treating patients at destinations other than EDs (e.g. urgent care centers, etc.) and for treating patients at the scene without further transport (see CMS diagram below).
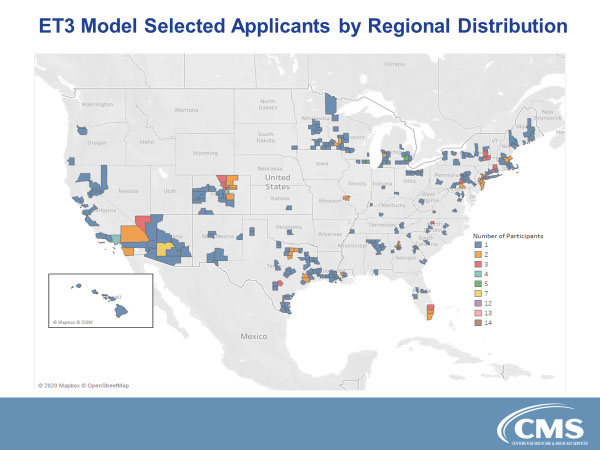
Recently, 205 agencies were accepted into the pilot (see CMS map below). Some are scheduled to begin providing service as soon as May 2020 and the rest within six months after that. A further ET3 pilot will examine the ability of emergency medical triage/dispatch centers to impact ED use before an ambulance is even dispatched by assessing calls and providing alternative services where appropriate.
Continue to read more on rural and urban EMS provision in the Days of ET3 and COVID-19 – in PART 2 on opportunities and lessons here.
 Kevin McGinnis, MPS, Paramedic Service Chief (Ret.) has been an EMS system builder since 1974. He is the communications technology advisor for five national EMS associations, and program manager for public safety communications, rural EMS and community paramedicine for the National Association of State EMS Officials (NASEMSO).
Kevin McGinnis, MPS, Paramedic Service Chief (Ret.) has been an EMS system builder since 1974. He is the communications technology advisor for five national EMS associations, and program manager for public safety communications, rural EMS and community paramedicine for the National Association of State EMS Officials (NASEMSO).
He received undergraduate and graduate degrees from Brown University and Cornell University in health care delivery systems and hospital administration. Kevin has been a paramedic, a paramedic service chief for volunteer, private, and hospital-based services, a hospital emergency department director, and Maine’s state EMS director.
He is the past Chairman of the U.S. Department of Homeland Security’s SafeCom Program and continues to serve on its Executive Committee. Kevin is Vice-Chair of the Governing Board of the National Public Safety Telecommunications Council and was bestowed its top honor, the Richard DeMello Award, in 2017.
Kevin has been an energetic promoter of the nationwide public safety broadband network since 2006. In August, 2015, he was named by the U.S. Secretary of Commerce to a second three-year term on the First Responder Network Authority (FirstNet) Board of Directors and termed out in October, 2018. He currently serves as the NASEMSO representative to the FirstNet Public Safety Advisory Committee. In 2018, Kevin received the Journal of EMS “Top Ten Innovator Award” for his FirstNet work. He was named by the Government Technology/Solutions for State and Local Government magazine as one of its 2013 “Top 25 Doers, Dreamers & Drivers in Public-Sector Innovation”.


